Critical Biomarker Omega-3 Index Not Increased by Healthy Eating
“I don’t take fish oil because I eat grass-fed beef and fish once a week,” my client said.
I told her that backstory about my experience selling omega-3 index testing to doctors a decade ago. (Scroll down for the full story.)
Back then, doctors and I found that even “real food” eating patients had suboptimal fatty acid levels—at least those living in Colorado, myself included at the time.
Which is why I’ve since been a fan of testing omega-3 levels and supplementing with fish oil.
For example, raising your omega-3 index from just three to six percent has been linked to serious cardiovascular disease risk reduction, among other health improvements, according to ample research. (1)
For optimal cardiovascular, metabolic and brain health, one’s omega-3 index ideally should be between eight and 12 percent.
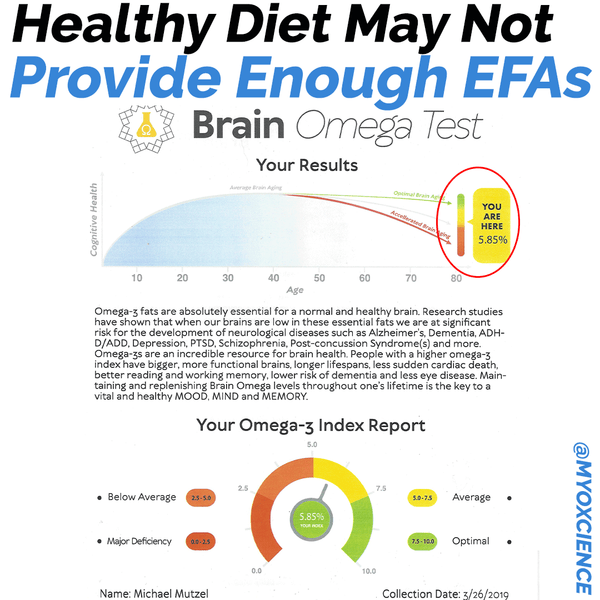
To put my own diet to the test, on January 1st I stopped taking our Myoxcience monoglyceride fish oil and retested my omega-3 index at the end of March.
The results came back at a low 5.6 percent (half of what is considered optimal).
Here’s an image of the actual test:
So, all the omega-3s from eggs laid by our pasture-raised chickens plus grass-fed beef and Northwest wild-caught salmon kept me just outside the critically low zone but put me short of optimal.
(Admittedly, we don’t eat much salmon in the winter, but still I thought my levels would be higher than six percent!)
For less than $50, you too can test your omega-3 index levels. Here are more details.
Omega-3 Index Testing: a review of the recent data
Reading time: 4 minutes
Outline:
-My history selling omega-3 index testing
-Why you should care about your omega-3 index
-Recent studies
When I was living in Boulder, CO, back in 2009, I hosted a seminar with Mark Houston, MD. SpectraCell labs was a co-sponsor of the event, and I was very impressed with their advanced lipoprotein particle testing technology (using the analytical ultracentrifugation technique under a test they called Lipoprotein Particle Profile or LPP). Per Robert Superko, pundit in the cholesterol lipoprotein particle testing space, the SpectraCell LPP test was the most accurate assessment of atherogenic (heart-disease promoting) particles at the time. Also at the time, Superko was a consultant for SpectraCell’s competitor at Berkeley Heart Lab, which used a gradient gel electrophoresis technology to assess lipoprotein particles. Berkeley was later acquired by Quest Diagnostics, a major lab testing company.
So when SpectraCell offered me job as a consultant to help functional medicine doctors use more accurate cardiovascular assessments in their patients, I gladly took it.
Below is a screenshot of the Journal of Circulation article published by Superko that I used to sell SpectraCell LPP tests to doctors after they hired me as a rep. Needless to say, this article also references the shortcomings of the NMR and VAP lipoprotein testing technologies, which, sadly, many doctors still use today.
Soon after I started selling the advanced cholesterol lipoprotein particle testing technology in January 2010, SpectraCell partnered with Omega Quant, offering Bill Harris’s Omega-3 Index Testing technology.
The Omega-3 Index quantifies the proportion of EPA and DHA in red blood cell membranes. It was a brilliant move on their end—as they already had the patient’s blood that they needed to to run the LPP, so why not also capture the patient’s omega-3 index and include it on the same report.
As a sales rep, this was an easy sell. I would simply show doctors the image below, which illustrates how the relative risk (RR) of sudden cardiac death (SCD) decreases when the composition of red blood cell EPA and DHA levels, or omega-3 index, increases from 3% to over 6%.
Since many doctors were already recommending omega-3 fatty acid supplements (fish oil) to doctors, this test allowed them to actually detect an omega-3 “insufficiency” for the first time. (Although a reduction in serum triglycerides associated with fish oil supplementation was, and still is, a common biomarker already used by many functional medicine doctors.)
If doctors were not convinced by that data, I would continue educating them about Harris’s findings, showing that an omega-3 index over 8% is linked with a 90% reduction in sudden cardiac death. (2) To my surprise, a few doctors were slow to implement this new testing technology and opted to continue to use archaic, standard cholesterol tests—largely because they didn’t want to change their in-office protocols or were getting kickbacks from the manufacturer.
New studies have shown that higher levels of omega-3 fatty acids were also associated with lower mortality in patients with heart failure and depression. (2)
When it comes to heart health, the data for increasing omega-3 fatty acid status is quite compelling, with four controlled trials of nearly 40,000 participants randomized to receive eicosapentaenoic acid (EPA) with or without docosahexaenoic acid (DHA) in studies of patients in primary prevention, after myocardial infarction, and most recently, with heart failure (HF).

Figure 2. Early benefit of omega-3 polyunsaturated fatty acid (-3 PUFA) therapy on total mortality, sudden death, coronary heart disease (CHD) mortality, and cardiovascular mortality. Probability measurements represent relative risk (95% confidence interval).
Source: Marchioli R, Barzi F, Bomba E, et al., for the GISSI-Prevenzione Investigators. Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI)-Prevenzione. Circulation 2002;105: 1897–903.
References
1) Harris, W. S. (2007). Omega-3 fatty acids and cardiovascular disease: a case for omega-3 index as a new risk factor. Pharmacological Research, 55(3), 217–223. http://doi.org/10.1016/j.phrs.2007.01.013
2) Wulsin, L. R., Blom, T. J., Durling, M., Welge, J. A., DelBello, M. P., Adler, C. M., et al. (2018). Cardiometabolic risks and omega‐3 index in recent‐onset bipolar I disorder. Bipolar Disorders, 20(7), 658–665. http://doi.org/10.1111/bdi.12633
RECENT POSTS
CATEGORIES
- 5-MTHF
- Adrenals
- air quality
- Berberine
- Blood Work
- caffeine
- Collagen
- Cortisol
- Creatine
- D-chiro-inositol
- Detoxification
- DHEA
- Electrolytes
- epigenetics
- Erythritol
- Exercise
- Fast Mimicking
- Fasting
- Fat Loss
- fires
- Glutathione
- GLY-NAC
- Glycine
- gut bacteria
- Hormones
- IFOS
- Inositol
- INTERNATIONAL FISH OIL STANDARDS (IFOS) PROGRAM
- Iodine
- longevity
- magnesium
- Magnesium L Threonate
- Metabolic Health
- Microbiome
- minerals
- Monk Fruit
- Multivitamin
- myo-inositol
- N-acetyl cysteine
- NAC
- omega-3 index
- Post exercise
- Pre Workout
- Recipe
- Sleep
- Stevia
- vitamin
- Vitamin B12
- Vitamin D
- Weight Loss
- whey protein
- Women's Health
- Zinc
- Zinc Taste Test